Developing Superpowers and Getting Ahead of Uncertainty
Uncertainty is profoundly uncomfortable. As a species, humans are hardwired to seek stability and predictability. We are so driven to avoid uncertainty that many people prefer a known negative outcome over an unknown one that could offer a better advantage. When we find ourselves in times of significant change—especially when a new presidential administration signals a major shift from historic norms—it challenges even those of us who are usually comfortable navigating ambiguity.
With such extensive change and so many unknowns, many leaders instinctively wait for greater clarity before taking action. After all, why invest in strategies that might quickly become obsolete? But waiting is itself a decision—and often a costly one. A passive "wait and see" approach not only risks missing emerging threats but also overlooks opportunities to mitigate or adapt to them. This mindset assumes stability will eventually return when, in reality, continuous change is more likely. It also underestimates the power leaders have to shape outcomes even in uncertain times. The longer organizations delay, the more likely they are to fall into a reactive, crisis-driven mode rather than a proactive, strategic one.
I recognize that change is disruptive, and the risks ahead are real. I do not mean to gloss over fear, risk, or the weight of difficult decisions. Each deserves attention, unfiltered and unvarnished. Yet, as leaders, our role is to remain agile and resilient—finding ways to fulfill our organizations' missions no matter how the future unfolds. This moment may push us into unfamiliar and challenging terrain, but it also presents a chance to—dare I say it?—uncover new opportunities.
Rather than being paralyzed by uncertainty, organizations can turn how they deal with uncertainty into a superpower. This superpower is built through three key steps: anticipating the unknown, strengthening resilience through near-term action, and building emotional connection, support, and alignment.
1. Anticipating the Unknown
The past two weeks have sent shockwaves through the healthcare industry, with major policy shifts being tested and signaled that could impact coverage, funding, reimbursement models, regulatory ground rules, and more. Should some of the policies and tenets shared through public discourse come to effect, they represent a radical transformation of the healthcare landscape. This is occurring at the same time as other critical challenges, such as workforce shortages, inflationary pressures, and the impact of AI and emerging technologies.
While the full picture remains in flux, organizations can piece together the variables already in motion—examining the likely pressure points, identifying where disruptions could emerge, and assessing how different policy, economic, and technological shifts could interact. This work can be informed by historical experience, but also to anticipate new ground altogether.
Playing out a scenario is different than a what-could-happen brainstorming session. The scenario framework fosters a richer view of possibilities and intersections. It also makes the future feel more visceral and real, unlocking fresh thinking. As possibilities emerge, we often find that there are more ‘no-brainer’ interventions that are meaningful across multiple or all scenarios. This leads to immediate ‘unsticking’.
There is also value in exploring where scenarios diverge. These offer a set of guard-rails that provide parameters of what is meaningful to explore. Anticipating risks, potential actions and opportunities in each of these futures makes a leadership team respond with greater readiness and agility should the scenario come to fruition. But more, the advanced thinking lays pathways for how to lead with a proactive and constructive reaction to change of any kind.
OUTCOME: The future feels less uncertain, and leaders gain a sense of control by identifying key variables, defining strategic responses, and establishing guideposts for potential policy and market shifts.
2. Strengthening Resilience Through Near-Term Actions
Change does not happen all at once. While some policy shifts unfold gradually, others can take effect with little warning, requiring organizations to be adaptable in real time. The act of scenario planning is not just about modeling various futures—it also exposes immediate steps that organizations can take to build resilience along the way.
By identifying key pressure points, leadership teams can put structures in place to manage uncertainty more effectively. Some examples of near-term interventions could include forming a rapid response committee to quickly assess and act on emerging developments, increasing the frequency and focus of employee and stakeholder communications to ensure alignment, or proactively investing in analysis and planning resources to strengthen the organization’s ability to react with agility. These actions create a level of preparedness that allows organizations to remain steady and responsive, even in unpredictable conditions.
OUTCOME: Organizations strengthen their ability to remain resilient through uncertainty by implementing near-term actions that reduce disruption, improve coordination, and enhance decision-making.
3. Building Emotional Connection, Support, and Alignment
Navigating change is not just a technical or operational challenge—it is deeply emotional. Periods of uncertainty can create anxiety, disengagement, and misalignment, especially when there is no shared sense of direction and employees lack clarity on how key issues could impact them. But when organizations engage in forward-looking discussions, something powerful happens: creative engagement fosters emotional connection, collective support emerges through shared commitment, and alignment improves as teams develop a common way of thinking about the future.
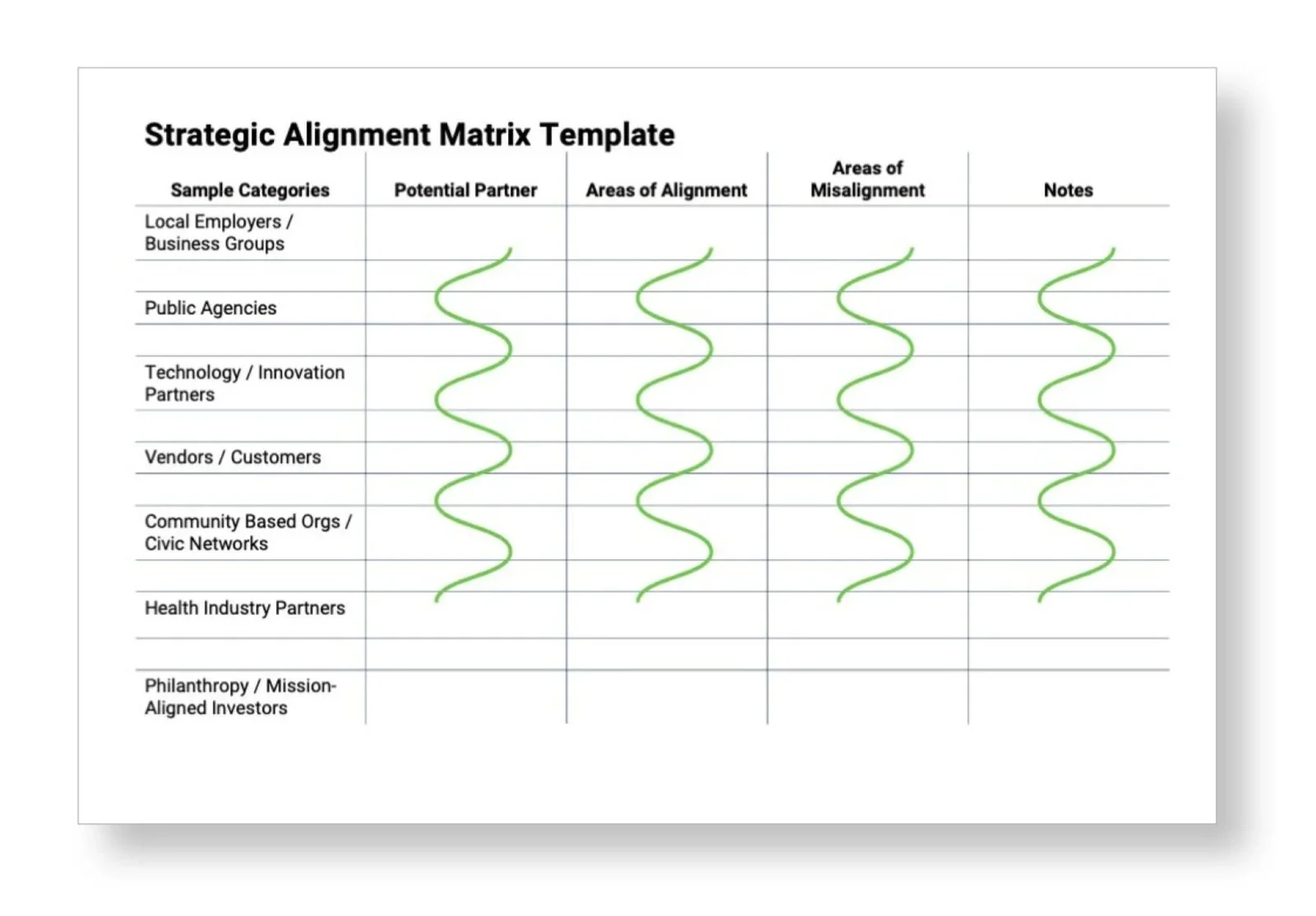
Through structured discussions and collaborative scenario exercises, leadership teams gain insight into areas of both alignment and misalignment, reducing friction and fostering more open, productive conversations. Leaders can see where perspectives diverge, uncover potential blind spots, and proactively address differences before they become roadblocks. At the same time, engaging in these discussions creates a shared narrative about what the future might hold, giving the entire organization a common language for thinking forward.
This level of transparency also strengthens trust. Employees see that leadership is not simply reacting to external forces but actively working through challenges in a thoughtful, structured way. With regular updates, they feel included and respected, which fosters a greater sense of shared purpose and reduces fear. When teams trust that leadership is making decisions with foresight and inclusivity, they are more likely to stay engaged, aligned, and committed to navigating change together.
OUTCOME: Organizations cultivate deeper emotional connection, shared commitment, and alignment—reducing friction, strengthening trust, and creating a common language for navigating the future together.
Putting on the Cape
Uncertainty is likely to remain a constant. Organizations that embrace preparation, resilience, and proactive leadership can turn how they deal with uncertainty into a superpower. The ability to anticipate change, align teams, and take decisive action is what sets them apart.
This mindset isn’t about ignoring real fears or concerns. In fact, leaning into them—acknowledging challenges while staying agile and forward-thinking—is part of the superpower we are building. It fosters trust, deepens alignment, and strengthens our ability to lead through uncertainty. By doing this strategic work in uncertain times, we’re not just managing risk—we’re embracing a fresh approach to addressing near-term challenges and also creating new possibilities for the future.
How is your organization managing uncertainty? Would love to swap tales.
With you in goodness,
NW